Total Pregnancy Solutions:
What is antenatal care?
Antenatal care is the care you receive from healthcare professionals during your pregnancy. You’ll be offered a series of appointments with your obstetrician.
He will check that you and your baby are well, give you useful information to help you have a healthy pregnancy (including healthy eating and exercise advice) and answer any questions you may have.
To give you the best pregnancy care, your doctor will ask you many questions about your health, your family’s health and your preferences. Your doctor will do some checks and tests, some of which will be done throughout your pregnancy. The results of these tests may affect your choices later in pregnancy, so it’s important not to miss them.
Your first visit
Your first visit with your doctor is the appointment when you tell them that you’re pregnant. At this first visit, you will be given information about:
- folic acid and vitamin D supplements
- nutrition, diet and food hygiene
- lifestyle factors that may affect your health or the health of your baby, such as smoking, recreational drug use and drinking alcohol
- antenatal screening tests
They will give you information on keeping healthy, and ask whether you have had any previous health or pregnancy issues, such as complications in pregnancy. It’s important to tell your doctor if:
- You’ve had any complications or infections in a previous pregnancy or delivery, such as pre-eclampsia or premature birth.
- You’re being treated for a chronic disease, such as diabetes or high blood pressure.
- You or anyone in your family have previously had a baby with an abnormality, such as spina bifida.
- There’s a family history of an inherited disease, such as sickle cell or cystic fibrosis.
An important part of antenatal care is getting information that will help you to make informed choices about your pregnancy. Your doctor will give you information in writing or some other form that you can easily use and understand.
Questions you might be asked The doctor might ask about:
- the date of the first day of your last period your health
- any previous illnesses and operations
- any previous pregnancies and miscarriaes
- ethnic origins of you and your partner, to find out whether your baby is at risk of certain inherited conditions, or other relevant factors, such as whether your family has a history of twins
- your job or your partner’s job, and what kind of accommodation you live in to see whether your circumstances might affect your pregnancy
how you’re feeling and whether you’ve been feeling depressed

Later antenatal visits
- Later visits are usually quite short. Your midwife or doctor will:
- check your urine and blood pressure
- feel your abdomen (tummy) to check the baby’s position
- measure your uterus (womb) to check your baby’s growth
- listen to your baby’s heartbeat if you want them to
You can also ask questions or talk about anything that’s worrying you. Talking about your feelings is as important as all the antenatal tests and examinations.
Checking your baby’s development and wellbeing
At each antenatal appointment from 24 weeks of pregnancy, your doctor will check your baby’s growth. To do this, they’ll measure the distance from the top of your womb to your pubic bone. The measurement will be recorded in your notes.
In the last weeks of pregnancy, you may also be asked to keep track of your baby’s movements. If your baby’s movements become less frequent, slow down or stop, contact your doctor immediately. You’ll be offered an ultrasound scan if they have any concerns about how your baby is growing and developing.
Routine antenatal tests
During your pregnancy, you’ll be offered a range of tests, including blood tests and ultrasound scans. These tests are designed to check for anything that may cause a problem during your pregnancy or after the birth, check and assess your wellbeing and your baby’s development and wellbeing, as well as screen for particular conditions.
Weight and height
Your height and weight are used to calculate your BMI (body mass index). Women who are overweight for their height are at increased risk of problems during pregnancy.
Most women put on 10-12.5kg in pregnancy, most of it after they are 20 weeks pregnant. Much of the extra weight is due to the baby growing, but your body also stores fat for making breast milk after the birth. During your pregnancy, it’s important to eat the right foods and do regular exercise.
Urine
You’ll be asked to give a urine sample at your antenatal appointments. Your urine is checked for several things, including protein or albumin. If this is found in your urine, it may mean that you have an infection that needs to be treated. It may also be a sign of pre-eclampsia.
Blood pressure
Your blood pressure will be taken at every antenatal visit. A rise in blood pressure later in pregnancy could be a sign of pregnancy-induced hypertension. It’s very common for your blood pressure to be lower in the middle of your pregnancy than at other times. This isn’t a problem, but it may make you feel lightheaded if you get up quickly.

Blood tests
As part of your antenatal care you’ll be offered several blood tests. Some are offered to all women, and some are only offered if you might be at risk of a particular infection or inherited condition. All the tests are done to check for anything that may cause a problem during your pregnancy or after the birth, or to check that your baby is healthy, but you don’t have to have them if you don’t want to.
Talk to your doctor and give yourself enough time to make your decision. Below is an outline of all the tests that can be offered.
Full Blood Count
Blood group
It is useful to know your blood group in case you need to be given blood, for example if you have heavy bleeding (haemorrhage) during pregnancy or birth. The test tells you whether you are blood group rhesus negative or rhesus positive. Women who are rhesus negative may need extra care to reduce the risk of rhesus disease (see below).
Rhesus (Rh) factor
Most people have a substance in their blood called the Rh factor. Their blood is called Rh positive. On average 17 people out of a 100 people don’t have the Rh factor – so their blood is called Rh negative. If your blood is Rh negative, it isn’t usually a problem, unless your baby happens to be Rh positive. If it is, there’s a risk that your body will produce antibodies against your baby’s blood.
People who are rhesus positive have a substance known as D antigen on the surface of their red blood cells. Rhesus negative people do not. A rhesus negative woman can carry a baby who is rhesus positive if the baby’s father is rhesus positive. If a small amount of the baby’s blood enters the mother’s bloodstream during pregnancy or birth, the mother can produce antibodies against the rhesus positive cells (known as ‘anti-D antibodies’).
This usually doesn’t affect the current pregnancy, but if the woman has another pregnancy with a rhesus positive baby, her immune response will be greater and she may produce a lot more antibodies. These antibodies can cross the placenta and destroy the baby’s blood cells, leading to a condition called rhesus disease, or haemolytic disease of the newborn. This can lead to anaemia and jaundice in the baby.
Anti-D injections can prevent rhesus negative women from producing antibodies against the baby. Rhesus negative mothers who haven’t developed antibodies are therefore offered anti-D injections at 28 and 34 weeks of pregnancy, as well as after the birth of their baby. This is quite safe for both the mother and the baby.
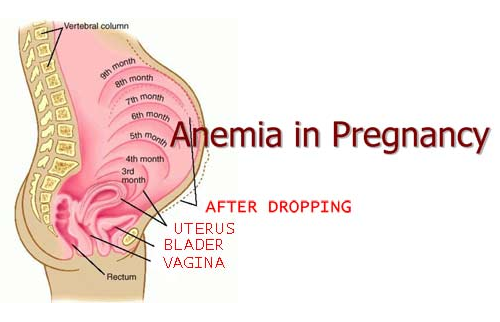
Anaemia
It is very common for women to develop iron deficiency during pregnancy. This is because your body needs extra iron so your baby has a sufficient blood supply and receives necessary oxygen and nutrients. Increasing the amount of iron- rich food you consume during your pregnancy can help avoid iron deficiency anaemia. Some pregnant women require an iron supplement, particularly from the 20th week of pregnancy. Anaemia makes you tired and less able to cope with any blood loss during labour and birth.
Your doctor can tell you if you need iron tablets to prevent or treat anaemia. Your iron levels will be checked throughout your pregnancy.
Infections
You’ll be offered tests for:
- Susceptibility to rubella (German measles) – if you get rubella in early pregnancy, it can seriously damage your unborn baby. Your midwife or doctor will talk to you about what happens if your test results show low or no immunity.
- Syphilis – you’ll be tested for this sexually transmitted infection as it can lead to miscarriage and stillbirth if left untreated.
- Hepatitis B – this virus can cause serious liver disease, and it may infect your baby if you’re a carrier or you’re infected during pregnancy. Your baby won’t usually be ill but has a high chance of developing long-term infection and serious liver disease later in life. Your baby can be immunised at birth to prevent infection. If you have hepatitis B, you’ll be referred to a specialist.
- Hepatitis C – this virus can cause serious liver disease and there is a small risk it will pass to your baby if you are infected. It can’t be prevented at present. If you’re infected, you’ll be referred to a specialist and your baby can be tested after it’s born
- HIV (human immunodeficiency virus) – this is the virus that causes AIDS. HIV infection can be passed to a baby during pregnancy, at delivery or after birth by breastfeeding. As part of your routine antenatal care, you’ll be offered a confidential test for HIV infection. If you’re HIV positive, both you and your baby can have treatment and care that reduces the risk of your baby becoming infected.
Be aware that you can still catch all these infections during pregnancy after you’ve had a negative test result. This includes sexually transmitted infections such as syphilis, HIV and hepatitis B if you or your sexual partner take risks, such as having unprotected sex. You can also get HIV and hepatitis if you inject drugs and share needles.
More about HIV
If you think that you’re at risk of getting HIV or you know that you’re HIV positive, talk to your doctor about HIV testing and counselling.
If you’re HIV positive, your doctor will need to discuss the management of your pregnancy and delivery with you.
There is a one-in-four chance of your baby being infected if you and your baby don’t have treatment. Treatment can significantly reduce the risk of transmitting HIV from you to your baby. One in five HIV-infected babies develop AIDS or die within the first year of life, so it’s important to reduce the risk of transmission.
Your labour will be managed in order to reduce the risk of infection to your baby. This may include an elective caesarean delivery.
Your baby will be tested for HIV at birth and at intervals for up to two years. If your baby is found to be infected with HIV, paediatricians can anticipate certain illnesses that occur in infected babies and treat them early. All babies born to HIV positive mothers will appear to be HIV positive at birth, because they have antibodies from their mother’s infection. If the baby is not HIV positive, the test will later become negative because the antibodies will disappear.
You’ll be advised not to breastfeed as HIV can be transmitted to your baby in this way.
Gestational diabetes
Gestational diabetes (GDM) is a type of diabetes that affects some women during pregnancy. Diabetes is a condition where there is too much glucose (sugar) in the blood.
Normally, the amount of glucose in the blood is controlled by a hormone called insulin. However, during pregnancy, some women have higher than normal levels of glucose in their blood and their body does not produce enough insulin to transport it all into the cells. This means that the level of glucose in the blood rises. Between 2 and 10 per cent of pregnant women will develop GDM.
In most cases, gestational diabetes develops in the third trimester (after 28 weeks) and usually disappears after the baby is born. However, women who develop gestational diabetes are more likely to develop type 2 diabetes later in life.
Pap test (smear test)
The Pap smear is a simple procedure to find early warning signs that cancer might develop in the future.
It is recommended that every woman presenting for antenatal care should be offered cervical screening by Pap smear if they have not had cervical screening within the past two years.
Pap smears can generally be undertaken during pregnancy, ideally before 24 weeks gestation. You many have some spotting and minor bleeding following the Pap smear. Your doctor should be able to advise you what is normal following a Pap smear and address any specific concerns you may have about having a Pap smear during pregnancy.

It’s okay to ask questions
It’s good to ask questions. Asking questions helps you understand more about your care. Remember that it’s your right to be fully informed about any tests or treatment you’re asked to have
You might want to ask your doctor:
- is this test/treatment routine in pregnancy
- how does it work
- why do I need it
- what are the benefits to me or my baby
- are there any risks to me or my baby
- do I have to have it
- what happens next if the results of a test are positive? What happens if they are negative?
- what are the chances of the test result being wrong (a false negative or a false positive)?
Write your questions down and take to your next appointment.
Group B streptococcus
Group B streptococcus (GBS, or group B strep) is a bacteria carried by up to 30% of people but it rarely causes harm or symptoms. In women it’s found in the intestine and vagina and causes no problem in most pregnancies. In a small number of pregnancies, it infects the baby, usually just before or during labour, leading to serious illness.
If you’ve already had a baby who had a GBS infection, you should be offered antibiotics during labour to reduce the chances of your new baby getting the infection. If you have had a group B streptococcal urinary tract infection with GBS (cystitis) during the pregnancy, you should also be offered antibiotics in labour.
GBS infection of the baby is more likely to occur if:
- your labour is premature (before 37 weeks of pregnancy)
- your waters break early
- you have a fever during labour
- you currently carry GBS.
Your doctor will assess whether you need antibiotics during labour to protect your baby from being infected. It’s possible to be tested for GBS late in pregnancy, if you have concerns talk to your doctor.